Clinical Skills Training & Simulation Center
The OUWB Clinical Skills Training & Simulation Center, or “Practice Clinic,” was formerly the site of the Beaumont Troy Family Medicine clinic.
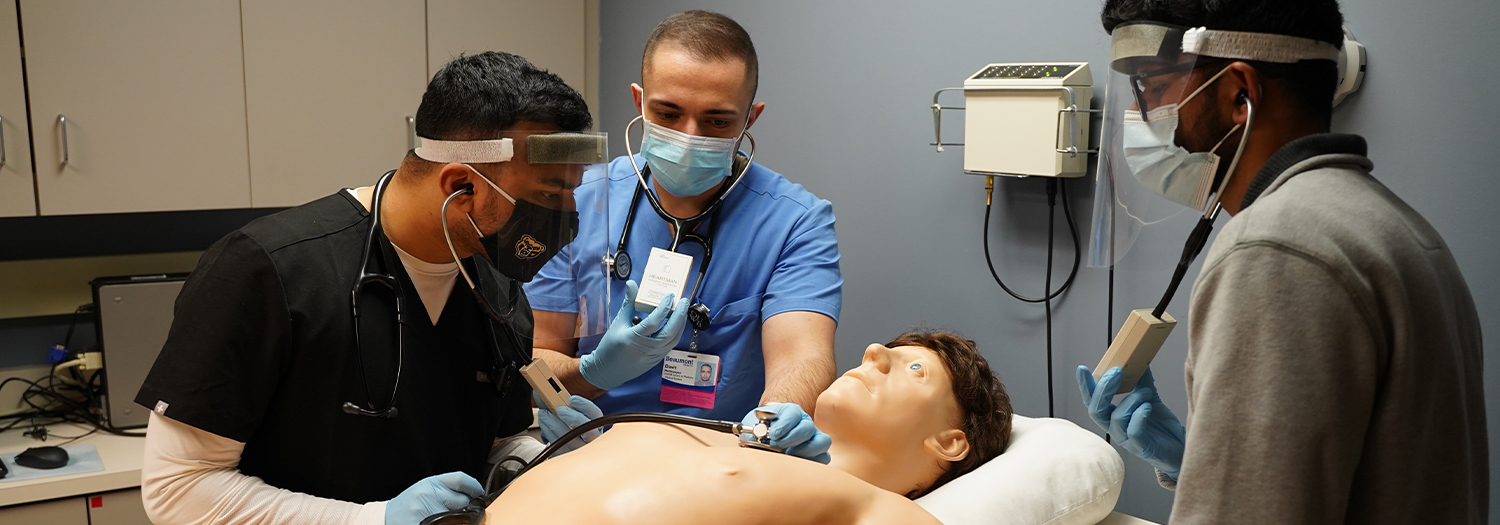
The Clinical Skills Training & Simulation Center is equipped to appear identical to a typical Family Medicine clinic. Additionally, each of the 16 exam rooms is equipped with video cameras, computer workstations in and outside each room and two-way communication with the master control station.
Students from all four years of medical school participate in clinical skills activities. This includes instruction, practice, and testing in interviewing and physical examination. Much of this instruction is conducted using Standardized Patients, persons trained to realistically simulate actual patients.
A "Harvey Heart Sounds” cardiovascular training mannequin is a key element of instruction in the examination of the cardiovascular system. With the touch of a button, the Harvey mannequin can be programmed to realistically portray myriad combinations of physical exam findings, each consistent with a specific condition or diagnosis.
What is a Standardized Patient?
A Standardized Patient (SP) is a layperson trained to present a clinical scenario just like a “real” patient for teaching or testing. SPs work at the OUWB Clinical Skills Center.
What are Standardized Patients (SPs) used for?
Students learn to interview/examine patients and gather information needed to help diagnose their problems. Students also:
- practice effective interpersonal skills to better communicate with patients
- learn appropriate techniques and approaches for physical examination of patients
- learn techniques to counsel patients in a variety of circumstances on a variety of issues
- gain experience with challenging issues such as breaking bad news
To learn more about becoming a standardized patient, please see our frequently asked questions.
Key characteristics of Standardized Patients:
- Growth mindset.
- Learner-centered.
- Reliable and punctual.
- Desire to contribute to the training process of excellent future physicians.
- Desire to help students progress through coaching and constructive feedback.
- Capacity to learn patient cases, coaching and feedback strategies, and evaluation processes.
- Ability to portray a patient case repeatedly with fidelity.
- Ability to evaluate student performance with reliability.
- Ability to gain proficiency in various technology platforms.
- Comfortable wearing a hospital gown.
- Comfortable with non-invasive physical exam maneuvers.
- Comfortable being videotaped for educational purposes.
- Comfortable with medical issues and working with health professional trainees.
- Maintains confidentiality of all student and case information.
- Strong written and verbal communication and interpersonal skills.
- Support OUWB's mission for diversity, equity, inclusion and belonging.
Casual Employment
- All SPs are casual employees of OUWB.
- Working hours are subject to change and fluctuate based on the needs of the programs.
- Casual employment is irregular and assignments are offered as needed. There is no expectation that there will be regular assignments or guaranteed hours.
Scheduling
- Student events are in person, Monday-Friday, between the hours of 8am and 6pm.
- SP events are scheduled based on the students' curricular schedules.
- Event dates will be provided 4-6 weeks in advance. Specific event times are subject to change based on student and program needs.
- Standardized Patients have the flexibility to accept or decline assignments based on personal needs.
Training
- Training is a hybrid model of in-person and remote learning.
- You will be trained to standardize the portrayal of a scripted patient case, medical history, family and social history, the patient’s behavior and emotional state, and how to simulate findings while being examined to ensure all students experience the same learning, feedback, and assessment.
- You will be trained to provide constructive feedback and evaluate student performance, based on the program goals and course objectives.
- You may also be trained to coach students on physical exam technique.
- You must be proficient in working with multiple tech platforms.
Compliance
- Complete a background check.
- Adhere to OUWB’s vaccine policies.
- Adhere to Beaumont Health mask policies.
Starting Wage: $15/hour
Additional questions can be directed to [email protected].
Troy Beaumont
Clinical Skills Training & Simulation Center
44300 Dequindre Road, 1st Floor,
Sterling Heights, MI 48314
Phone: (248) 964-5198

